Attorney General Dave Yost | Official website
Attorney General Dave Yost | Official website
In a series of indictments filed this month, Ohio Attorney General Dave Yost's office has accused 13 Medicaid providers of defrauding the government healthcare program. Twelve home-health aides and one behavioral-health specialist are alleged to have billed Medicaid for services totaling $189,332 that were not provided. These actions have resulted in felony charges of Medicaid fraud and theft. The Medicaid Fraud Control Unit conducted investigations leading to these indictments in Franklin County Common Pleas Court.
"Billing for made-up services checks every box for fraud, waste and abuse," Yost stated. "Medicaid fraud steals from the vulnerable and from the taxpayers who fund the program – and we don’t tolerate that in Ohio."
The announcement coincides with the U.S. Department of Justice's 2025 National Health Care Fraud Takedown, which brought criminal charges against 324 defendants nationwide for health-care fraud and illegal drug-diversion schemes involving $14.6 billion in false billings.
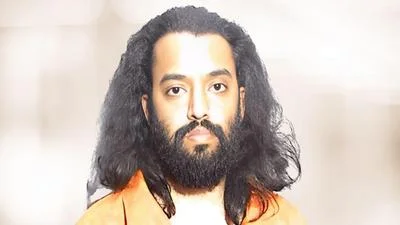
Among those indicted on state charges is a Cleveland resident accused of billing Medicaid while a service recipient was out of the country, resulting in a $64,316 loss. Other cases include allegations ranging from falsifying time sheets to billing for services while traveling or working other jobs.
Ohio’s Medicaid Fraud Control Unit collaborates with federal, state, and local partners to combat Medicaid fraud and protect vulnerable adults. The unit investigates healthcare providers who defraud the state Medicaid program and enforces patient abuse laws.
Indictments represent criminal allegations; defendants are presumed innocent unless proven guilty in court.
The Ohio Medicaid Fraud Control Unit receives funding primarily from the U.S. Department of Health and Human Services, supplemented by the Ohio Attorney General’s Office.





 Alerts Sign-up
Alerts Sign-up