Attorney General Dave Yost | Official website
Attorney General Dave Yost | Official website
Indictments have been filed against 16 Medicaid providers in Ohio, accusing them of collectively stealing $1.7 million from the government health-care program. The cases were investigated by the Medicaid Fraud Control Unit, part of the office of Ohio Attorney General Dave Yost, and brought before the Franklin County Common Pleas Court.
“Medicaid fraud may be a financial crime, but it comes at a human cost,” said Attorney General Yost. “It preys on the vulnerable who depend on the program and betrays the trust of the taxpayers who fund it.”
The indicted individuals include two people previously convicted of felonies who were prohibited from providing services to Medicaid recipients but still received hundreds of thousands of dollars through improper billing. Other cases involve providers accused of billing for home health services while clients were hospitalized or while they themselves were out of state.
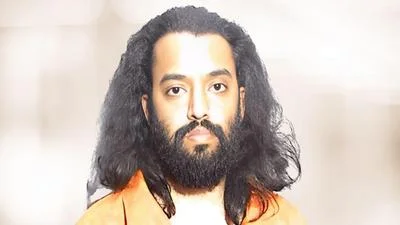
Among those charged is an individual from Ashtabula who had been convicted of murder in West Virginia in 1998 and was therefore ineligible to be a Medicaid provider. Despite this restriction, his employers billed Medicaid $230,936 for his services after an investigation began with a tip about billing for unrendered services.
Another case involves a 67-year-old from Akron with convictions for involuntary manslaughter and felonious assault, who was found to have illegally billed $4,633 as a home health care provider.
A 39-year-old from Eastlake faces charges including aggravated theft and Medicaid fraud after allegedly billing for services when clients were hospitalized between January 2022 and June 2025. Investigators reported that this resulted in an $819,400 loss to Medicaid. Three associates also face indictments related to this case.
Other individuals are accused of overbilling or submitting fraudulent timesheets for services not rendered. One home health aide allegedly billed for care while on a cruise from Los Angeles to Hawaii, initially claiming her patient accompanied her before investigators presented travel records and social media evidence.
The Ohio Medicaid Fraud Control Unit operates within the Health Care Fraud Section and works with federal, state, and local partners to investigate fraud and protect vulnerable adults. The unit prosecutes healthcare providers who defraud Medicaid and enforces laws related to patient abuse and neglect.
Funding for the unit comes primarily from federal sources: 75% is provided by the U.S. Department of Health and Human Services under a grant totaling $15,343,488 for fiscal year 2025; the remaining 25%, amounting to $5,114,493 for FY 2025, is funded by the Ohio Attorney General’s Office.
As stated in official communications, indictments are criminal allegations; all defendants are presumed innocent unless proven guilty in court.





 Alerts Sign-up
Alerts Sign-up